Purpose
To reveal differences or advantages in regard to different treatment options after proton beam therapy for uveal melanoma.
Design
Retrospective, comparative, interventional case series.
Methods
All patients receiving intravitreal treatment between January 2011 and July 2014 for radiation maculopathy after proton beam therapy were included. Excluded were all patients who required re-irradiation, vitrectomies, or tumor resections; and those whose treatment was performed for potentially other reasons, such as radiation-induced optic neuropathy, or where visual outcome was influenced by tumor growth under the macula or macular ischemia. Minimum follow-up was 12 months after last injection.
Results
Of 78 patients, 38 (48.7%) received bevacizumab injections, 35 (44.9%) triamcinolone acetonide injections, and 5 (6.4%) a dexamethasone implant. In the bevacizumab group visual acuity improved in 11 patients (28.9%) by 0.25 logMAR (0.1–0.4 logMAR) and remained stable in 24 patients (63.2%) 4 weeks after injection. In the triamcinolone group visual acuity showed improved outcomes in 10 patients (28.6%) by 0.25 logMAR (0.1–0.4 logMAR) and stability in function in 20 patients (57.1%). Four weeks after dexamethasone implantation visual acuity remained stable in 4 patients (80%). No differences among the groups were detected regarding functional outcome or reduction in central foveal thickness.
Conclusions
This study showed that antiangiogenic or corticosteroid intravitreal treatment led to reduced central foveal thickness and visual improvement in some patients without showing differences or advantages. Therefore a patient-specific treatment choice can be recommended.
Ever since the COMS Study, priority has been given to eye-preserving irradiation modalities. Because of adequate local tumor control and subsequent eye retention rates, visual outcome has become an area of great interest. Visual outcome is often compromised because of complications resulting from irradiation. Such complications are irradiation retinopathy, maculopathy, and/or optic neuropathy. To date, a common consensus concerning the best treatment for radiation maculopathy has not been reached yet. Studies reporting on intravitreal injections, either with corticosteroids after brachytherapy or with anti–vascular endothelial growth factor (anti-VEGF) agents after external beam and brachytherapy treatment, all showed promising results in reducing foveal thickness and improving visual acuity. This study reveals, retrospectively, if there are differences or advantages in regard to different treatment options after proton beam therapy for choroidal or ciliary body melanoma.
Methods
Inclusion and Exclusion Criteria
The retrospective, comparative, interventional case series was approved by the institutional review board of the Charité-Universitätsmedizin Berlin, Berlin, Germany, and was performed in accordance with the tenets of the Declaration of Helsinki. A total of 134 charts of patients presenting with uveal melanoma receiving intravitreal treatment between January 2011 and July 2014 were reviewed. Inclusion criteria consisted of the diagnosis of choroidal or ciliary body melanoma treated with primary proton beam therapy, the occurrence of proton beam–associated radiation maculopathy with verified macular edema in optical coherence tomography (OCT), an intravitreal treatment with only 1 drug for radiation maculopathy, and a minimum follow-up of 12 months after last injection. All included patients had undergone proton beam therapy with a dose of 60 cobalt gray equivalent in total (cobalt gray equivalent: 1 cobalt gray equivalent = 1.1 gray, taking a radiobiological effectiveness of 1.1 into account), given in 4 fractions of 15 cobalt gray equivalent on 4 sequential days.
Excluded were all patients who required re-irradiation, vitrectomies, or tumor resections. Further excluded were those who received intravitreal treatment combined with other surgical procedures or in whom the etiology of macular edema could not be clarified owing to potential influence of previous surgeries, diabetes, or age-related macular degeneration. Furthermore, those whose treatment was performed for potentially other reasons, such as radiation-induced optic neuropathy, or in whom visual outcome was influenced by tumor growth under the macula or macular ischemia (defined as >180-degree enlargement of the foveal arcade) were identified by fluorescein angiography at the time of detecting radiation maculopathy.
Main Outcome Measures
Main outcome measures were defined as differences in applied drugs regarding changes in central foveal thickness on OCT using Spectralis (Heidelberg Engineering, Heidelberg, Germany) and visual outcome. Best-corrected-visual acuity (BCVA), central foveal thickness on OCT, and, when available, fluorescein angiography (Heidelberg Engineering) were evaluated at initial diagnosis of radiation maculopathy. Besides information of central foveal thickness in micrometer (μm), macular edema was furthermore classified as resolved, reduced (reduction of more than 10 μm in central foveal thickness), stable, and increased (increase of more than 10 μm in central foveal thickness).
Secondary Outcome Measures Reported in Subgroup Analysis
Secondary outcome measures were defined as changes or differences regarding enlargement of the foveal avascular zone. Owing to inconsistently performed fluorescein angiographies at baseline visits, we included only those patients who underwent, at minimum, 2 fluorescein angiographies—before treatment and during further follow-up—for subgroup analysis. Furthermore, patients with inconsistent intravitreal therapy were excluded from the study and were analyzed separately in another subgroup analysis.
Statistical Methods
Statistical analysis was performed using SPSS 20.0 (SPSS, Inc, Chicago, Illinois, USA). The Kolmogorov-Smirnov test and the Shapiro-Wilk test were used for testing normality. To detect potential initial differences among the 3 groups, a Kruskal-Wallis test was performed. Per analysis of covariance, the influence of radiation doses to fovea and optic disc on functional outcome, OCT, and fluorescein angiography changes was tested. A Wilcoxon-Mann-Whitney test was used to find differences in non–normally distributed variables. A Fisher exact test was used to detect interrelationships between the clinical grading of macular edema on OCT according to treatment groups; χ 2 test and factorial analysis of variance were used to assess statistically significant differences between groups. Interrelationships between variables were assessed by calculating correlation coefficients according to Spearman/Pearson. Visual acuity is described as logMAR. In relation to the MARAN protocol, light perception (LP) was added as 2.1 logMAR, hand motion (HM) as 2.0 logMAR, and counting fingers (CF) as 1.9 logMAR.
Results
Patient Demographics
In total, 78 patients were included for analysis of the main outcome measures of visual acuity and central foveal thickness. Of these patients, 38 (48.7%) received 1.25 mg in 0.05 mL bevacizumab injections, 35 (44.9%) received 4 mg in 0.1 mL triamcinolone acetonide injections, and 5 (6.4%) received a dexamethasone implant. Mean patient age was 59 (range, 34–74) years, 61 (range, 27–81) years, and 69 (range, 60–77) years for patients treated with bevacizumab, triamcinolone acetonide, and dexamethasone, respectively. Median tumor thickness was 3.1 mm (range, 1.2–14.1 mm), 3.5 mm (range, 1.4–11.6 mm), and 2.9 mm (range, 2.3–4.4 mm) in the bevacizumab, triamcinolone acetonide, and dexamethasone group, respectively. Median largest basal diameter was 10.0 mm (range, 4.3–20.8 mm) in the bevacizumab group, 10.3 mm (range, 5.8–21.9 mm) in the triamcinolone acetonide group, and 11.3 mm (range, 7.6–12.3 mm) in the dexamethasone group. Tumor volume was 141 mm 3 (range, 9–2535 mm 3 ), 158 mm 3 (range, 25–1735 mm 3 ), and 139 mm 3 (range, 72–236 mm 3 ); median distance to fovea was 0.9 mm (range, 0–11.0 mm), 2.1 mm (range, 0–12.0 mm), and 1.6 mm (range, 0–3.7 mm); and distance to optic disc was 2.6 mm (range, 0–11.0 mm), 1.5 mm (range, 0–14.7 mm), and 2.3 mm (range, 0–2.7 mm) in patients receiving bevacizumab, triamcinolone acetonide, and dexamethasone implant, respectively.
Kruskal-Wallis test revealed no statistically significant differences between the groups in age (χ 2 = 3.551, P = .169), tumor thickness (χ 2 = 0.274, P = .872), largest basal diameter (χ 2 = 1.156, P = .561), volume (χ 2 = 0.537, P = .765), distance to fovea (χ 2 = 4.095, P = .129), distance to optic disc (χ 2 = 2.531, P = .282), initial visual acuity (χ 2 = 4.993, P = .82), and central foveal thickness before injection (χ 2 = 0.673, P = .769). Therefore groups were defined to be homogenous and comparable ( Table 1 ).
| Treatment Option | P Value (Kruskal-Wallis-Test) | |||
|---|---|---|---|---|
| Bevacizumab | Triamcinolone Acetonide | Dexamethasone Implant | ||
| Number (%) of patients (N = 78) | 38 (48.7%) | 35 (44.9%) | 5 (6.4%) | |
| Mean age in years (range) | 59 (34–74) | 61 (27–81) | 69 (60–77) | .169 |
| Median tumor thickness in mm (range) | 3.1 (1.2–14.1) | 3.5 (1.4–11.6) | 2.9 (2.3–4.4) | .872 |
| Median largest basal diameter in mm (range) | 10.0 (4.3–20.8) | 10.3 (5.8–21.9) | 11.3 (7.6–12.3) | .561 |
| Median tumor volume in mm 3 (range) | 141 (9–2535) | 158 (25–1735) | 139 (72–236) | .765 |
| Median distance to fovea in mm (range) | 0.9 (0–11.0) | 2.1 (0–12.0) | 1.6 (0–3.7) | .129 |
| Median distance to optic disc in mm (range) | 2.6 (0–11.0) | 1.5 (0–14.7) | 2.3 (0–2.7) | .282 |
| Median initial visual acuity in logMAR (range) | 0.1 (0–1.3) | 0.2 (0–0.7) | 0.2 (0–0.3) | .82 |
| Median visual acuity before injection in logMAR (range) | 0.8 (0–2.0) | 0.8 (0.1–2.0) | 0.8 (0.2–1.3) | .780 |
| Median visual acuity at 4 weeks after injection in logMAR (range) | 0.7 (0.1–2.0) | 0.8 (0.1–2.0) | 0.8 (0.2–1.3) | .871 |
| Median central foveal thickness in μm before injection (range) | 479 (248–1123) | 454 (156–957) | 440 (226–589) | .769 |
| Median central foveal thickness in μm at 4 weeks after injection (range) | 362 (134–836) | 314 (138–940) | 265 (142–534) | .757 |
Follow-up and Important Intervals
In all patients (n = 78), the median observation period from the time of proton beam therapy to final follow-up visit was 49 months (range, 18.1–120.0 months). Radiation maculopathy with increased central foveal thickness on OCT occurred on average 16.6 months (range, 4.6–69.3 months) following proton beam therapy. The symptom/treatment interval was defined as the interval between detection of radiation maculopathy and first injection and was on average 4.5 weeks (range, 0.5–10 weeks).
Visual Acuity According to Group and Further Limiting Complication of Optic Neuropathy
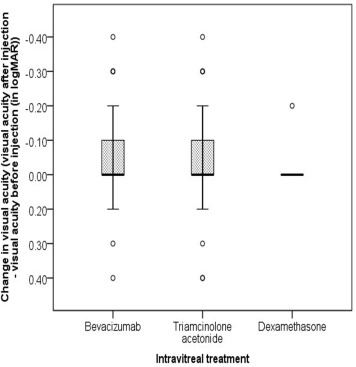
Visual acuity changes by group are summarized in Figures 1 and 2 .
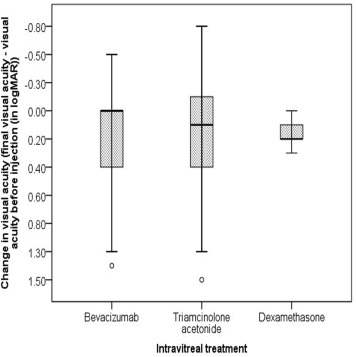
Bevacizumab group
On average, 2 injections (range, 1–11 injections) were administered and median time between initial detection of macular edema and first intravitreal injection was 5 weeks (range, 0.5–8 weeks). Median initial visual acuity was 0.1 logMAR (range, 0–1.3 logMAR) before proton beam therapy. Median visual acuity at time of diagnosis of radiation maculopathy was 0.5 logMAR (range, 0–1.5 logMAR). Furthermore, median visual acuity was 0.8 logMAR (range, 0–2.0 logMAR) before injection and 0.7 logMAR (range, 0.1–2.0 logMAR) 4 weeks following last injection. Final visual outcome was 1.0 logMAR (range, 0.1–2.0 logMAR), with 10 patients (26.3%) maintaining visual acuity of 0.5 logMAR or better.
Visual acuity improved in 11 of 38 patients (28.9%), on average by 0.25 logMAR (range, 0.1–0.4 logMAR); remained stable in 24 patients (63.2%); and decreased in 3 patients (7.9%), by 0.1 logMAR (range, 0.1–0.3 logMAR), upon visual acuity assessment 4 weeks after last injection. When measured at last follow-up, compared with values before injection, median visual outcomes showed long-term improvement in 6 patients (15.8%), by 0.2 logMAR (range, 0.05–0.3 logMAR); stability in 13 patients (34.2%); and deterioration in 19 patients (50%), by 0.3 logMAR (range, 0.1–0.5 logMAR).
Radiation optic neuropathy affecting long-term visual outcome
Twelve of the 38 bevacizumab patients (31.6%) developed radiation optic neuropathy 18 months (range, 2–35 months) after last injection. Long-term visual outcome was slightly affected, although without any statistically significant difference. While patients without optic neuropathy presented with final visual outcomes of 1.0 logMAR (range, 0.3–2.0 logMAR), patients with radiation optic neuropathy showed poorer outcomes of 1.1 logMAR (range, 0.1–1.9 logMAR).
Triamcinolone acetonide group
Triamcinolone acetonide was administered, on average, as a single dose (range, 1–3 injections), and median symptom/treatment interval (the time between first detection of macular edema and first intravitreal injection) was 4 weeks (range, 0.5–9.5 weeks). Patients presented with median visual acuity of 0.2 logMAR (range, 0–0.7 logMAR) before proton beam therapy, 0.6 logMAR (range, 0–1.5 logMAR) upon diagnosis of radiation maculopathy, 0.8 logMAR (range, 0.1–2.0 logMAR) before injection, 0.8 logMAR (range, 0.1–2.0 logMAR) 4 weeks after last injection, and 1.0 logMAR (range, 0.2–2.1 logMAR) at last follow-up. Final visual acuity of 0.5 logMAR or better was sustained in 9 of the 35 patients (25.7%).
Visual acuity showed improved outcomes in 10 patients (28.6%), by 0.25 logMAR (range, 0.1–0.4 logMAR), measured 4 weeks after last injection; and in 7 patients (20.0%), by 0.1 logMAR (range, 0.05–0.4 logMAR), at last follow-up, compared with visual acuity before injection. Stability in function was achieved in 20 (57.1%) and 6 (17.1%) patients after injection and at last follow-up, respectively. Decreased vision was detected in 5 patients (14.3%), by 0.1 logMAR (range, 0.05–0.3) 4 weeks after last injection; and in 19 patients (54.3%), by 0.3 logMAR (range, 0.1–0.8 logMAR), at last follow-up visit.
Radiation optic neuropathy affecting long-term visual outcome
Radiation optic neuropathy occurred in 15 of the 35 triamcinolone acetonide patients after 6 months (range, 2–24 months). Patients with radiation optic neuropathy also showed decreased final visual outcome of 1.2 logMAR (range, 0.2–2.1 logMAR), compared to 1.0 logMAR (range, 0.2–1.7logMAR) in patients without optic neuropathy. There was no statistically significant difference detected.
Dexamethasone implant group
The dexamethasone implant was injected, on average, once (range, 1–2 injections) after a median symptom/treatment interval of 4 weeks (range, 2–10 weeks). Patients who received a dexamethasone implant had visual acuity of 0.2 logMAR (range, 0–0.3 logMAR) before proton beam therapy. Median visual acuity at time of radiation maculopathy diagnosis was 0.5 logMAR (range, 0–1.3 logMAR). Median visual acuity before and after intravitreal injection was 0.8 logMAR (range, 0.2–1.3 logMAR). Final visual acuity was 1.0 logMAR (range, 0.4–2.0 logMAR) in 1 patient in whom visual acuity of 0.5 logMAR or better was maintained.
Four weeks after implantation, visual acuity remained stable in 4 patients and decreased in 1 patient, by 0.2 logMAR, compared with visual acuities before implantation. Comparing last follow-up visual acuity with visual acuity before implantation, 1 patient remained stable, whereas visual acuity decreased in 4 patients, by 0.2 logMAR (range 0.1–0.3 logMAR).
Radiation optic neuropathy affecting long-term visual outcome
One of the 5 dexamethasone implant patients developed radiation optic neuropathy 2 months after injection, exhibiting a final visual acuity of 0.7 logMAR.
Optical Coherence Tomography
Analysis of OCT scans showed a significant reduction ( P < .05) in foveal thickness in each of the 3 groups, comparing central foveal thickness (in micrometers) at date of radiation maculopathy diagnosis with central foveal thickness 4 weeks after intravitreal treatment. After bevacizumab injection, a decrease was observed from 479 μm (range, 248–1123 μm) to 362 μm (range, 134–836 μm) ( P = .01). After triamcinolone acetonide administration, a decrease was detected from 454 μm (range, 156–957 μm) to 314 μm (range, 138–940 μm) ( P = .034), and after dexamethasone implant injection, there was a decrease from 440 μm (range, 226–589 μm) to 265 μm (range, 142–534 μm) ( P = .049). There was no statistically significant difference among the groups according to intravitreal treatment.
Of 78 patients, 25 (32.1%) showed completely resolved macular edema 4 weeks after last injection, 32 (41.0%) showed reduced macular edema, 11 (14.1%) had stable macular edema, and 10 (12.8%) exhibited increased macular edema ( Table 2 ). Final visual acuities were statistically significantly better in patients who presented with resolved macular edema than with reduced, stable, or increased macular edema (bevacizumab group: P = .046, triamcinolone acetonide group: P = .05) ( Table 3 ).
| Macular edema | Treatment Option | Total | ||
|---|---|---|---|---|
| Bevacizumab | Triamcinolone Acetonide | Dexamethasone Implant | ||
| Resolved | ||||
| N | 11 | 12 | 2 | 25 |
| % | 28.9% | 34.3% | 40.0% | 32.1% |
| Reduced | ||||
| N | 15 | 14 | 3 | 32 |
| % | 39.5% | 40.0% | 60.0% | 41.0% |
| Stable | ||||
| N | 5 | 6 | 0 | 11 |
| % | 13.2% | 17.2% | 0,0% | 14.1% |
| Increased | ||||
| N | 7 | 3 | 0 | 10 |
| % | 18.4% | 8.5% | 0,0% | 12.8% |
| Macular edema | Treatment Option | ||
|---|---|---|---|
| Bevacizumab | Triamcinolone Acetonide | Dexamethasone Implant | |
| Resolved | |||
| N | 11 | 12 | 2 |
| VA preinj. | 0.5 (0–1.4) | 0.65 (0.3–1.3) | 0.85 (0.4–1.3) |
| VA 4 weeks | 0.4 (0–1.4) | 0.5 (0.2–1.0) | 0.75 (0.2–1.3) |
| Final VA | 0.5 (0.1–1.9) a | 0.75 (0.2–2.0) b | 1.0 (0.7–1.3) c |
| Reduced | |||
| N | 15 | 14 | 3 |
| VA preinj. | 0.8 (0.3–1.3) | 1.0 (0.1–2.0) | 0.8 (0.2–1.0) |
| VA 4 weeks | 0.7 (0.3–1.3) | 1.0 (0.1–1.9) | 0.8 (0.2–1.0) |
| Final VA | 1.0 (0.3–1.3) | 1.0 (0.3–1.6) | 1.0 (0.3–1.0) |
| Stable | |||
| N | 5 | 6 | 0 |
| VA preinj. | 1.3 (0.8–2.0) | 1.1 (0.6–1.5) | |
| VA 4 weeks | 1.3 (0.8–2.0) | 1.1 (0.8–1.7) | |
| Final VA | 1.5 (0.7–2.0) | 1.25 (1.0–1.7) | |
| Increased | |||
| N | 7 | 3 | 0 |
| VA preinj. | 0.5 (0.3–1.5) | 0.6 (0.4–2.0) | |
| VA 4 weeks | 0.8 (0.5–1.5) | 1.0 (0.4–2.0) | |
| Final VA | 1.3 (0.5–1.5) | 1.3 (0.4–2.1) | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


