Purpose
To evaluate changes in anterior chamber depth (ACD) and angle width after neodymium–yttrium-aluminum-garnet (Nd:YAG) laser capsulotomy.
Design
Prospective interventional case series.
Methods
In a single institution, 43 eyes of 43 consecutive pseudophakic patients with symptomatic posterior capsule opacification (PCO) underwent Nd:YAG laser capsulotomy. Anterior chamber depth and angle width in pseudophakic eyes with posterior capsule opacification were measured with anterior segment optical coherence tomography (AS-OCT) before and 3 days after Nd:YAG laser capsulotomy. Preoperative and postoperative measurements of anterior chamber depth and angle width included the angle opening distance, measured as the perpendicular distance from the trabecular meshwork at 500 μm and 750 μm anterior to the scleral spur to the anterior iris surface (AOD500 and AOD750, respectively), and anterior chamber angle (ACA) in the nasal and temporal quadrants. Main outcome measures were the changes in ACD and angle width parameters.
Results
The mean patient age was 63.4 ± 3.6 years. Before Nd:YAG laser capsulotomy, mean ACD, AOD500, AOD750, and ACA (nasal and temporal) measurements were 3.71 ± 0.11 mm, 0.61 ± 0.054 mm, 0.67 ± 0.063 mm, and 34.5 ± 1.67 degrees and 34.8 ± 1.55 degrees, respectively. Three days after Nd:YAG laser capsulotomy, mean ACD, AOD500, AOD750, and ACA (nasal and temporal) measurements were 3.77 ± 0.1 mm, 0.69 ± 0.06 mm, 0.73 ± 0.06 mm, and 35.51 ± 1.64 degrees and 36.17 ± 1.51 degrees, respectively ( P < .01 for all).
Conclusions
The depth and width of the ACA in pseudophakic eyes with PCO increased significantly after Nd:YAG laser capsulotomy, as shown by AS-OCT, a reliable and noncontact method for measuring anterior ocular structures. Our study shows that the different angle parameters such as ACD, AOD500, AOD750, and ACA measurements seem highly correlated.
Anterior segment cross-sectional imaging is a valuable method to evaluate anterior chamber configuration quantitatively. Recently, anterior segment optical coherence tomography (AS-OCT), a noninvasive and noncontact method, has emerged as a new imaging technique for anterior ocular structures. It provides high-resolution images by using a long wavelength (1310 nm) of light; it offers rapid quantitative analysis of various structures. AS-OCT has demonstrated good repeatability and reproducibility with low intra-observer and inter-observer variability. One limitation of AS-OCT is its incomplete penetration through the pigmented epithelium of the iris; thus, it is difficult to obtain accurate images of the ciliary body, lens, and zonules behind the pigmented iris.
Posterior capsule opacification (PCO), one of the most common complications of cataract surgery, can reduce visual acuity and contrast sensitivity, as well as cause glare or monocular diplopia. Neodymium–yttrium-aluminum-garnet (Nd:YAG) laser capsulotomy is the gold-standard treatment for PCO. Several studies report conflicting results in anterior chamber depth (ACD) and angle width after Nd:YAG laser capsulotomy because different methods were used. Using ultrasound biometry, Thornval and Naeser in 1995, Hu and associates in 2000, and Özkurt and associates in 2009 did not find significant changes in ACD after Nd:YAG posterior capsulotomy. However, Zaidi and Askari in 2004 found a decrease in ACD, whereas Findl and associates observed an increase in ACD after Nd:YAG posterior capsulotomy.
The object of this study was to analyze changes in ACD and angle width after Nd:YAG laser capsulotomy using AS-OCT, a recent and more sophisticated method for measuring anterior ocular structure parameters.
Methods
This study included 43 eyes of 43 consecutive pseudophakic patients with symptomatic PCO (22 female, 21 male) who presented for Nd:YAG laser posterior capsulotomy at Medipol University School of Medicine, Department of Ophthalmology between November 11, 2013 and February 21, 2014. The study used an interventional case series design. Patients who underwent uncomplicated phacoemulsification surgery with a hydrophobic square-edged posterior chamber intraocular lens (IOL) (Alcon IQ; Alcon, Fort Worth, Texas, USA) at least 6 months prior to posterior capsulotomy and who experienced PCO that deteriorated visual acuity were included in the study. The mean time between posterior capsulotomy and cataract surgery was 19.16 ± 6.99 months (range: 6–37 months).
Eyes lacking clear corneas or those having posterior segment pathologies were excluded. Patients with glaucoma, previous intraocular surgery other than uneventful phacoemulsification, ocular trauma, or other intraocular pathology, or who were unable to understand the study or communicate, were excluded. The study protocol was approved by the Ethics Committee of Medipol University. The tenets of the Declaration of Helsinki were followed and all patients provided informed consent prior to enrollment.
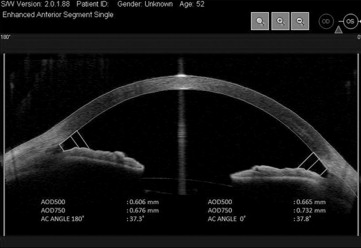
All patients underwent routine ophthalmic examinations including visual acuity, Goldmann tonometry, slit-lamp biomicroscopy, and funduscopy before and 3 days after Nd:YAG laser capsulotomy. Refractive errors were measured as manifest refraction. The AS-OCT measurements were performed by 2 experienced technicians before and 3 days after the Nd:YAG laser capsulotomy using a Visante AS-OCT device (Carl Zeiss Meditec, Inc, Dublin, California, USA). Technicians were masked to clinical ophthalmic examination results. For the measurements, pupils were undilated and patients were asked to sit and fixate on an indicator in the AS-OCT under identical lighting conditions. Images of the nasal and temporal angle quadrants (0 degree and 180 degree meridians) were captured until the centration and quality were sufficient for analysis. The best images were selected and analyzed using custom software (Iridocorneal Module; Carl Zeiss Meditec, Inc) to detect changes by Nd:YAG laser capsulotomy over ACD and anterior chamber angle (ACA).
All Nd:YAG laser capsulotomies were performed using a Q-switched Nd:YAG laser (YC-1600; Nidek Co. Ltd, Gamagori, Japan) by the same surgeon (M.E.). The procedure was performed in 18 right eyes and 25 left eyes. After the procedure was explained and informed consent obtained, 1 drop of tropicamide 0.5% and 1 drop of phenylephrine 2.5% were instilled in each eye. Twenty to 30 minutes later, a standard Abraham capsulotomy lens was applied after topical application of oxybuprocaine hydrochloride 0.4% eye drops. The capsulotomy was fashioned in a cross pattern to create at least a 4-mm-diameter opening. Details of the number of laser pulses and energy used were recorded. The mean energy level used was 1.42 ± 0.17 mJ with a mean of 20 ± 11 laser pulses. After the procedure, topical apraclonidine 1%, timolol 0.5%, dexamethasone sodium phosphate, and diclofenac sodium 0.1% drops were instilled. Intraocular pressure was measured 1 hour after the procedure. Dexamethasone sodium phosphate and diclofenac sodium 0.1% drops, 4 times per day, were prescribed for 2 weeks.
ACD is defined as the distance from the endothelium to the anterior pole of IOL at the center of the cornea. We calculated ACA width by measuring the angle between the iris tangential line and the posterior corneal surface with its apex in the angle recess ( Figure 1 ). ACA width was also analyzed using standardized angle parameters after manual identification of the apex of the iris recess and scleral spur. Angle opening distances at 500 μm (AOD500) and AOD at 750 μm (AOD750) were measured as the perpendicular distances measured from the trabecular meshwork at 500 μm and 750 μm, respectively, anterior to the scleral spur to the anterior iris surface ( Figure 2 ).

All statistical analyses were performed using SPSS version 20 (SPSS Inc, Chicago, Illinois, USA). Using a paired t test, we compared preoperative and postoperative angle measurements and ACD. A Kolmogorov-Smirnov test was used to test for normality between samples, followed by a Levene test to assess equal variances. All P values were 2-sided and were considered statistically significant when <.05.
Results
The mean patient age was 63.4 ± 3.6 years (range: 56–72 years). The mean intraocular pressure was 16.3 mm Hg before capsulotomy and 18.9 mm Hg 3 days after capsulotomy, a 16% increase ( P < .001). Average axial length was 23.1 ± 0.85 mm (range: 21.30–25.24 mm).
The mean ACD values before and 3 days after capsulotomy were 3.71 ± 0.11 mm and 3.77 ± 0.10 mm, respectively ( Table ; P < .001). Changes in ACD and preoperative ACD were negatively correlated (r = −0.314, P < .01). All nasal and temporal angle values analyzed by AS-OCT significantly increased after capsulotomy ( Table ). The mean postcapsulotomy nasal angle increase was 0.97 degrees (widening of 2.8%) and temporal angle increase was 1.34 degrees (widening of 3.8%). The increase in ACA was negatively correlated with preoperative ACA for both nasal (r = −0.355, P < .05) and temporal (r = −0.364, P < .05) angles.
| Parameter | Mean ± SD | Mean Difference (95% CI) | P Value | |
|---|---|---|---|---|
| Before Laser Capsulotomy | After Laser Capsulotomy | |||
| ACD (mm) | 3.71 ± 0.17 | 3.77 ± 0.10 | 0.06 ± 0.04 | <.001 |
| ACA (degrees) | ||||
| Nasal | 34.54 ± 1.78 | 35.52 ± 1.65 | 1.06 ± 0.75 | <.001 |
| Temporal | 34.83 ± 1.56 | 36.18 ± 1.51 | 1.34 ± 0.58 | <.001 |
| AOD500 (mm) | ||||
| Nasal | 0.61 ± 0.05 | 0.70 ± 0.06 | 0.09 ± 0.02 | <.001 |
| Temporal | 0.63 ± 0.05 | 0.73 ± 0.06 | 0.01 ± 0.02 | <.001 |
| AOD750 (mm) | ||||
| Nasal | 0.67 ± 0.06 | 0.73 ± 0.06 | 0.06 ± 0.02 | <.001 |
| Temporal | 0.75 ± 0.06 | 0.85 ± 0.06 | 0.09 ± 0.01 | <.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


