Purpose
To evaluate the characteristics of aniseikonia in patients with rhegmatogenous retinal detachment (RD) after pneumatic retinopexy.
Design
Prospective, interventional case series study.
Methods
Thirty patients who had undergone pneumatic retinopexy as the initial procedure for rhegmatogenous retinal detachment were selected for this study. The principal outcomes included visual acuity, postoperative aniseikonia measured by the New Aniseikonia Test, anatomical success, and measurement of central retinal thickness using optical coherence topography (OCT). These outcomes were measured postoperatively at 3, 6, and 12 months.
Results
The median patient age was 37 years (range, 13–57 years), with 17 cases of macula-off RD and 13 cases of macula-on RD. All of these patients achieved anatomical success, proven by OCT after surgical repair. Three months after pneumatic retinopexy, 18 patients (60.0%) developed micropsic aniseikonia and aniseikonia was diagnosed in 15 patients (88.2%) in the macula-off RD group, leaving 2 patients (11.8%) unaffected. In the macula-on RD group, 3 patients (23.1%) were found to have aniseikonia, while 10 patients (76.9%) were unaffected. The presence of aniseikonia was strongly linked to the difference in central retinal thickness, between the operated eye and the fellow eye, measured at 12 months postoperatively.
Conclusion
Aniseikonia after pneumatic retinopexy for rhegmatogenous RD may be related to the preoperative macular status. Macula-off RD patients had a higher incidence of aniseikonia, compared to macula-on RD patients, following retina reattachment. There was a moderate to high correlation between the grading of aniseikonia and the difference in central retinal thickness.
Aniseikonia is a phenomenon in which the size or shape of perceived images differs between eyes. The anomaly is reported to be associated with interocular differences in refractive error (optically induced aniseikonia) and some retinal diseases (retinally induced aniseikonia). Following successful repair for rhegmatogenous retinal detachment, some patients have complained that objects appeared distorted in size or shape (dysmetropsia).
Rhegmatogenous retinal detachment (RD) is a vision-threatening condition, caused by the passing of liquefied vitreous through a retinal break into the potential epithelioretinal interspace between the sensory retina and the retinal pigment epithelium (RPE). Current treatment strategies for rhegmatogenous RD include scleral buckling (SB), vitrectomy, and pneumatic retinopexy. However, after treatment with scleral buckling, the axial length of the eyeball changes and this may affect the refractive status. Cataract formation is one of the most common sequelae after vitrectomy with gas tamponade, with cataract progression corresponding to changes in the refractive status. Changes in axial length and cataract formation are characteristics of optically induced aniseikonia. For the treatment of some particular types of rhegmatogenous RD, pneumatic retinopexy may be used, where pure gas is injected into the vitreous cavity, followed by postoperative positioning. The gas tamponades the retinal breaks until chorioretinal adhesion is complete. The advantages of pneumatic retinopexy include the simplicity of the procedure, no refractive shift, improved final visual acuity for macula-off detachments, and no loss of final visual acuity if the procedure fails. However, even though pneumatic retinopexy does not cause a refractive shift, some patients still complained of aniseikonia. The aim of this study was the characterization of aniseikonia, among patients with rhegmatogenous RD treated with pneumatic retinopexy.
Methods
This prospective, interventional case series consisted of consecutive patients with rhegmatogenous RD, treated with pneumatic retinopexy at Taichung Veterans General Hospital from December 2011 to December 2013. The protocol was approved prospectively by the Institutional Review Board of Taichung Veterans General Hospital (No: CE14200). This study was conducted in accordance with the Declaration of Helsinki. Thirty patients (15 men and 15 women) were enrolled in the study. Informed consent was obtained from all patients after an explanation of the nature and possible consequences of the study. The inclusion criteria were rhegmatogenous RD patients who had been treated by pneumatic retinopexy with steamroller technique, with no surgical complications, no changes in lens opacity, no aniseikonia before RD, and satisfactory retinal reattachment. The exclusion criteria were changes in lens opacity, refractive shift after pneumatic retinopexy (greater than 1 diopter), surgical complications, aniseikonia before RD, and retained subretinal fluid ( Figure 1 ). Patients with a refractive difference between the operated eye and the fellow eye greater than 1 diopter were also excluded. Patient data collected included age, sex, visual acuity (VA) in the Snellen system, lens status, macular status, intraocular pressure, refractive status, axial length, central retinal thickness, and results of the New Aniseikonia Test. All data were recorded before the operation and at 3, 6, and 12 months postoperatively, except for central retinal thickness and the New Aniseikonia Test results, which were recorded only postoperatively.
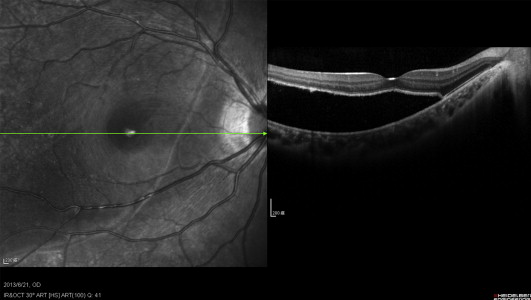
Lens status was graded by a board-certified ophthalmologist (K.H.L.) based on the Lens Opacities Classification System III (LOCS III). Central retinal thickness was measured by optical coherence tomography (Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany). The computerized New Aniseikonia Test was conducted according to the guidelines, as described by Ugarte and Williamson. The New Aniseikonia Test measures the ratio of image size difference between the 2 eyes. Patients were divided into 2 groups, aniseikonia group (where the size/shape of perceived images differed between eyes) and non-aniseikonia group (where the size/shape of perceived images did not differ between eyes). On the other hand, patients were also divided into macula-on RD group and macula-off RD group on the basis of the preoperative macular status.
Statistics
We compared age, duration of symptoms to operation time, visual acuity, differences in intraocular pressure (IOP), axial length, refraction, and central retinal thickness between the aniseikonia and the non-aniseikonia groups, using the Mann-Whitney U test. Statistical analyses were performed using SPSS software version 12.0 (SPSS, Inc, Chicago, Illinois, USA) and P values <.05 were considered statistically significant.
Results
The average age of the study patients was 37.60 ± 13.09 years, with a range of 13–57 years. The macula-off RD group included 17 patients and the macula-on RD group included 13 patients. Three months after pneumatic retinopexy, 18 patients (60.0%) had developed aniseikonia and all of them were micropsic. In the macula-off RD group, 15 patients (88.2%) had aniseikonia and 2 patients (11.8%) were not affected. In the macula-on RD group, 3 patients (23.1%) had aniseikonia while 10 patients (76.9%) remained unaffected. Aniseikonia after pneumatic retinopexy for rhegmatogenous RD was related to preoperative macular status. Macula-off RD patients had a far higher incidence of aniseikonia than did patients with macula-on RD following retina reattachment ( P < .01, Table 1 ).
| Macula-Off RD N = 17 | Macula-On RD N = 13 | |
|---|---|---|
| Aniseikonia, n (%) | 15 (88.2%) | 3 (23.1%) |
| Non-aniseikonia, n (%) | 2 (11.8%) | 10 (76.9%) |
Aniseikonia was not significantly related to age ( P = .851), duration of symptoms to operation time ( P = .158), difference in refractive status ( P = .491), or axial length ( P = .346) between the operated eye and the fellow eye. However, aniseikonia was significantly related to the difference in central retinal thickness between the operated eye and the fellow eye ( P = .035, Table 2 ).
| Non-Aniseikonia Patients, | Aniseikonia Patients, | P Value | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (y) | 37.67 ± 12.67 | 37.56 ± 13.73 | .851 |
| OP time (day) | 23.42 ± 31.4 | 22.00 ± 20.93 | .158 |
| VA diff. | 0.06 ± 0.018 | 0.11 ± 0.11 | .065 |
| Ref. diff. (Diopter) | −0.06 ± 0.62 | −0.07 ± 0.32 | .491 |
| IOP diff. (mm Hg) | 0.17 ± 1.47 | 0.33 ± 1.24 | .755 |
| AL diff. (mm) | −0.01 ± 0.21 | −0.07 ± 0.44 | .346 |
| CRT diff. (μm) | 9.75 ± 15.4 | 19.39 ± 17.36 | .035 |
The correlation between the grading of aniseikonia and the difference in central retinal thickness was measured by linear regression. These results showed a moderate correlation (Pearson correlation coefficients were −0.487 in the vertical meridian and −0.510 in the horizontal meridian) at 3 months after the operation ( Figure 2 ). This finding encouraged further investigation into the relationship between aniseikonia grading and differences in central retinal thickness at 6 months and 12 months after surgery. We found there was a moderate correlation (Pearson correlation coefficients were −0.674 in the vertical meridian and −0.609 in the horizontal meridian) at 6 months after surgery ( Figure 3 ); however, a high correlation (Pearson correlation coefficients were −0.732 in the vertical meridian and −0.743 in the horizontal meridian) was seen at 12 months after surgery ( Figure 4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


