Amblyopia
Jonathan M. Holmes BM, BCh
Michael X. Repka MD, MBA
Raymond T. Kraker MSPH
A number of multicenter randomized controlled trials (RCTs) and prospective observational studies have been conducted by groups in North America and Europe addressing questions in the treatment of amblyopia. The Pediatric Eye Disease Investigator Group (PEDIG) in the United States1 consists of approximately 200 pediatric ophthalmologists and pediatric optometrists across North America, in both academic and community-based private practice settings, who conduct large simple trials or simple data collection studies, each study mimicking clinical practice with the exception of randomization and standardized masked assessment of outcome measures. This chapter summarizes the major findings of completed PEDIG amblyopia studies2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17 and also describes several studies conducted by other investigator groups in Europe.18,19,20,21,22,23,24
To date, RCTs in amblyopia have exclusively addressed questions in the management of unilateral amblyopia caused by anisometropia, strabismus, or a combination of anisometropia and strabismus. No RCTs have been conducted in deprivation amblyopia, and therefore, this chapter will not discuss the management of deprivation amblyopia or bilateral amblyopia.
Visual Acuity Testing in Amblyopia Studies
The standardization and masking of visual acuity (VA) measurement are critical for clinical trials in amblyopia. The use of age-appropriate clinical tests that incorporate a logMAR scale is important for the analysis and presentation of results. For children aged <7 years, PEDIG uses the amblyopia treatment study (ATS) VA protocol,25 incorporating HOTV optotypes with surround bars. The test has been automated with a computer-based electronic visual acuity (EVA) tester.26 Many children under 3 years are untestable with HOTV optotypes,25 so PEDIG studies of younger children with amblyopia have focused on 3- to <7-year-olds. For children aged 7 years or more, PEDIG uses an EVA version of the early treatment of diabetic retinopathy study (ETDRS) test (the e-ETDRS test),27 presenting single optotypes with surround bars and yielding a letter score comparable to standard ETDRS testing. In the European studies, Clarke et al.,19 Stewart et al.,20,21,22,23,24 and Awan et al.18 also used logMAR-based VA tests for outcome assessment.
Atropine versus Patching in Moderate Amblyopia
Background and Study Questions
Historically, advocates of atropine administered to the fellow eye in the treatment of amblyopia have suggested that enhanced compliance and better binocular outcomes are advantages of atropine, while advocates of patching the fellow eye have suggested that patching produces a more complete and more rapid response. In order to address this controversy, the first RCT conducted by PEDIG compared patching of the fellow eye prescribed for at least 6 hours per day to atropine 1% one drop each morning to the fellow eye.2,9
Patients Included in the Study
Children were <7 years old at the time of enrollment and had to be able to complete optotype VA testing (HOTV matching), effectively limiting the study to 3- to <7-year-olds. They had moderate amblyopia defined as 20/40 to 20/100 in the amblyopic eye, fellow eye acuity of at least 20/40, and at least 3 logMAR lines of interocular difference to ensure that they had bona fide amblyopia. In addition, the presence or history of an amblyogenic (or more properly amblyopiogenic) factor that met criteria for strabismus, anisometropia, or both was required for enrollment. Patients could have had no more than 2 months of amblyopia therapy in the past 2 years and optimum spectacle correction (if needed) was required for at least 4 weeks.2
Intervention and Outcome Measures
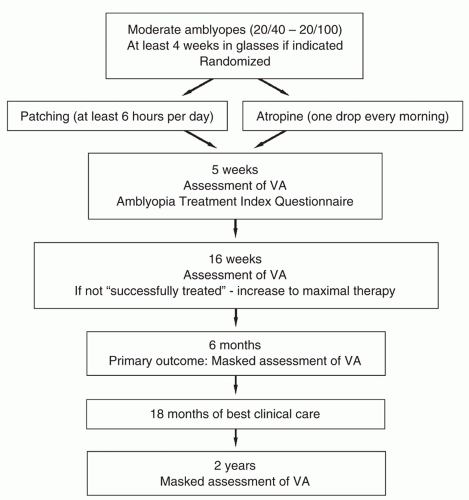
Randomization and follow-up schedule are shown in Figure 14.1. If the amblyopic eye had not improved by 3 lines or to at least 20/32 after 16 weeks of randomized treatment, the treatment was increased by either changing the spectacle lens over the fellow eye to plano in the atropine group or increasing the patching to 12 or more hours per day in the patching group.2
The primary outcome was best-corrected amblyopic eye VA measured 6 months from enrollment and randomization.2 After 6 months of treatment according to randomization, investigators were allowed to treat each patient at their discretion. A long-term follow-up examination was then conducted at 2 years from enrollment, at age 10 years, and further follow-up is being conducted at age 15 years.
Major Findings
At the 6-month primary outcome, both groups showed similar improvement in the amblyopic eye VA (a mean improvement of 3.16 lines in the patching group and 2.84 lines in the atropine group).2 The difference in VA between treatment groups was small— equivalent to approximately 1.5 letters—and not clinically meaningful (mean difference 0.034 logMAR units; 95% confidence interval [CI], 0.005 to 0.064). Improvement was initially faster in the patching group, with a mean improvement from baseline to 5 weeks of 2.22 lines in the patching group and 1.37 lines in the atropine group. Defining the 6-month outcome dichotomously as success or failure, with success defined as “20/32 or better in the amblyopic eye and/or improved from baseline by three or more lines,” success was achieved in 79% of the patching group and 74% of the atropine group, which was not statistically different. The relative treatment effect did not vary according to age, depth of amblyopia, or cause of amblyopia.2
Atropine had a slightly higher degree of acceptability when rated on a parental questionnaire28,29 administered at the 5-week visit, before knowledge of any VA improvement.
Between 6 months and 2 years following randomization,9 treatment was at the discretion of the investigator, but only about a quarter of the children underwent treatment using the other modality. At the 2-year outcome, the mean improvement in amblyopic eye VA was again similar in the patching and atropine groups (3.7 lines in the patching group and 3.6 lines in the atropine group). The difference in mean VA between the groups was very small (0.01 logMAR units; 95% CI, -0.02 and 0.04). In both groups, the mean amblyopic eye acuity at 2 years was approximately 20/32, 1.8 lines poorer than the mean fellow eye acuity, which was approximately 20/20. It is noteworthy that only about half of the patients in each group reached 20/25 or better in the amblyopic eye. There was no difference in stereoacuity between patients in the patching and atropine groups when assessed at the 2-year outcome.
At the 10-year-old examination,30 the mean amblyopic eye acuity, measured in 169 patients, was 0.17 logMAR (approximately 20/32) and 46% of amblyopic eyes were 20/25 or better. Mean amblyopic and fellow eye visual acuities at age 10 years were similar in the original treatment groups (p = 0.56 and 0.80, respectively). Examinations at age 15 years are ongoing and will be completed in the late summer 2013.
Implications for Clinical Practice
Both patching and daily atropine drops administered to the fellow eye are excellent initial treatments for moderate anisometropic and strabismic amblyopia. It is reasonable to involve the parents and the child in deciding which treatment to start. If that treatment modality is unsuccessful, the child could be put on the alternative therapy.
Unanswered Questions
The optimum dose of patching and dose of atropine were not addressed in this study. The doses used in this study were selected by consensus of the investigator group prior to initiating the RCT, and the patching dose was prescribed at the discretion of the investigator (starting with at least 6 hours per day in this study). Questions regarding optimum dose would begin to be addressed by studies described later in this chapter.
If a patient had not responded at 16 weeks to atropine therapy, the hypermetropic glasses correction over the fellow eye was reduced to a plano lens. This would have the effect of further blurring the VA of the cyclopleged fellow eye. Whether the use of a plano lens in addition to atropine results in increased effectiveness of treatment is being studied in a PEDIG RCT and will be described later in this chapter.
Analysis of fixation data and near VA data in patients randomized to atropine surprisingly revealed that fixation switch to the amblyopic eye was not necessary for VA improvement, and that patients who had better near VA in the fellow eye while under atropine cycloplegia could also show improvement in the amblyopic eye.31 For practical reasons, this assessment was limited by performing these tests at the 5-week visit. The issues of fixation switch and near VA predicting success with
atropine were also explored in the PEDIG RCT of atropine regimes, described later in the chapter.
atropine were also explored in the PEDIG RCT of atropine regimes, described later in the chapter.
At the outcomes 2 years from randomization9 and at 10 years of age,30 only about half the children improved to 20/25 or better. This indicates that amblyopia is difficult to “cure.” Future studies need to address the best treatment strategy for residual amblyopia and one such study is described later in this chapter. It is probable that a proportion of children with amblyopia have organic deficits that cannot be completely reversed by current treatment.
The role of optical treatment of amblyopia (termed “refractive adaptation” by some)22,24,32 with spectacles alone was not addressed in this trial. The choice of “at least 4 weeks in glasses, if needed” was made as a compromise between those who wanted to start patching or atropine immediately and those who wanted to wait for maximal improvement. Subsequent work of Moseley, Stewart, Fielder et al.22,24,32 has provided evidence that a great deal of improvement can be obtained with glasses alone in both strabismic and anisometropic amblyopia, in some cases eliminating the need for patching or atropine. Two studies of optical treatment of amblyopia are described.
Optical Treatment of Anisometropic Amblyopia
Background and Study Questions
In purely anisometropic amblyopia, it seems reasonable that correcting the refractive error alone might be enough to treat amblyopia, by providing a focused image to the retina of the amblyopic eye.
Patients Included in the Study
A total of 84 children 3 to <7 years old with previously untreated anisometropic amblyopia were enrolled with visual acuities ranging from 20/40 to 20/250.12
Intervention and Outcome Measures
In this nonrandomized prospective observational study,12 optimal refractive correction was provided and VA was measured with the new spectacle correction at baseline, confirming the presence of amblyopia and then measured at 5-week intervals until VA stabilized or amblyopia resolved. The main outcome measure was the maximum improvement in best-corrected VA in the amblyopic eye and proportion of patients whose amblyopia resolved.
Major Findings
Amblyopia improved with optical correction by 2 or more lines in 77% of the patients and resolved in 27%.12 Improvement took up to 30 weeks before stabilization criteria were met. Even after stabilization, additional improvement occurred with spectacles alone in 21 of 34 patients followed in a control group of a subsequent randomized trial, resolving in 6 patients. Treatment outcome was not related to age, but was associated with better baseline VA and lesser amounts of anisometropia.12
Implications for Clinical Practice
Refractive correction alone improves VA in most cases and results in resolution of amblyopia in about one-third of 3- to <7-year-old children with previously untreated anisometropic amblyopia. While most cases of resolution occur in those with moderate (20/40 to 20/100) levels of amblyopia, the nearly 3-line average improvement in VA resulting from initial treatment with spectacles alone may lessen the burden of subsequent therapy.12
Unanswered Questions
It is difficult to be certain that a case of presumed anisometropic amblyopia is purely anisometropic or whether there is a strabismic component. Some investigators suggest that most cases of anisometropic amblyopia have a small angle misalignment, and this is supported by recent evidence on lack of bifoveality in many cases of anisometropic amblyopia.33 In fact, it has been very recently suggested that the “microesotropia flick” seen in some cases of anisometropic amblyopia may represent fixation instability.34 Since there may be a contribution of strabismic amblyopia to cases of presumed anisometropic amblyopia, it raises the question of whether optical treatment has a role in strabismic and combined
strabismic-anisometropic amblyopia. This question is address next.
strabismic-anisometropic amblyopia. This question is address next.
Optical Treatment of Strabismic Amblyopia
Background and Study Questions
In the previous study, we also enrolled 12 children with strabismic amblyopia for optical treatment alone,12 as a run-in phase for a subsequent RCT. Surprisingly, we observed improvement in VA almost to the same degree as the children with purely anisometropic amblyopia.35 Amblyopia improved with optical correction by 2 or more lines in 9 of 12 (75%) of the patients and resolved in 3 (25%). We hypothesized that there might be two mechanisms explaining the improvement: 1) correction of blur that would place a focused image on the retina of the amblyopic eye, which might be beneficial despite apparent lack of fixation and 2) improvement of alignment, which might place the image on the fovea of the amblyopic eye. We addressed these questions in the following subsequent study.36
Patients Included in the Study
A total of 146 children 3 to <7 years old with previously untreated strabismic amblyopia (N = 52) or combined-mechanism amblyopia (N = 94) were enrolled in this prospective observational study.36
Intervention and Outcome Measures
Optical treatment was provided as spectacles (prescription based on a cycloplegic refraction, the full cylinder correction, and generally the full plus correction according to protocol) that were worn for the first time at the baseline visit.36 VA with spectacles was measured using the ATS HOTV VA protocol at baseline and every 9 weeks thereafter until no further improvement in VA. Ocular alignment was assessed at each visit. The main outcome measure was best-corrected VA 18 weeks after baseline.36
Major Findings
Overall, amblyopic eye VA improved a mean of 2.6 lines (95% CI, 2.3 to 3.0), with 75% of children improving ≥2 lines and 54% improving ≥3 lines.36 Resolution of amblyopia occurred in 32% (95% CI, 24% to 41%) of the children. The treatment effect was greater for strabismic amblyopia than for combined-mechanism amblyopia (3.2 vs. 2.3 lines, adjusted p = 0.003). VA improved regardless of whether eye alignment improved.36
Implications for Clinical Practice
Optical treatment alone of strabismic and combined-mechanism amblyopia results in clinically meaningful improvement in amblyopic eye VA for most 3- to <7-year-old children, resolving in at least one quarter of the children without the need for additional treatment.36 It is therefore reasonable to prescribe spectacles alone for children with strabismic and combined anisometropic-strabismic amblyopia, in addition to those with presumed anisometropic amblyopia.
Unanswered Questions
The mechanism for improvement of VA with optical correction alone for strabismic and combined anisometropic-strabismic amblyopia is not entirely clear. Since similar improvement occurred in eyes that remained strabismic with hypermetropic correction, we speculate that putting a focused image on the retina of the amblyopic eye contributes to the improvement, whether or not we can detect “fixation” with that eye on a clinical exam.
Additional Treatment Beyond Spectacles versus No Additional Treatment
Background and Study Questions
PEDIG conducted an RCT of “continued spectacles alone” versus “adding 2 hours of daily patching,” in children whose VA had stabilized on optical (spectacle) treatment.11
Patients Included in the Study
One hundred and eighty children 3 to < 7 years old with best-corrected amblyopic eye VA of 20/40 to 20/400 associated with strabismus, anisometropia, or both who had worn optimal refractive correction (if needed) for at least 16 weeks or for two consecutive visits without improvement11 were included in this study.
Intervention and Outcome Measures
Children were randomized either to 2 hours of daily patching with 1 hour of near visual activities or to continued spectacles alone (if needed). Patients were continued on the randomized treatment (or no treatment) until no further improvement was noted. The main outcome measure was best-corrected VA in the amblyopic eye after 5 weeks.11
Major Findings
Improvement in VA of the amblyopic eye from baseline to 5 weeks averaged 1.1 lines in the patching group and 0.5 lines in the control group (p = 0.006), and improvement from baseline to best measured VA with continued treatment beyond 5 weeks averaged 2.2 lines in the patching group and 1.3 lines in the control group (p < 0.001).11
Implications for Clinical Practice
This has been one of the few RCTs in amblyopia with an untreated control group, and the study showed that, following a period of optical treatment of amblyopia and after VA had stabilized, 2 hours of daily patching combined with 1 hour of near visual activities improves moderate to severe amblyopia in children 3 to <7 years old.
Unanswered Questions
Surprisingly, there was continued improvement in VA in the control group where we thought that maximum VA had already been reached following optical treatment of amblyopia. This suggests that the criteria for “stability” used in this study (no improvement in VA over 2 visits 5 weeks apart, or treatment for at least 16 weeks) and in clinical care were inadequate. Nevertheless, this does not detract from the primary finding of a benefit from 2 hours of daily patching, because this study was an RCT.
Prescribed Full-Time versus Prescribed Part-Time Patching in Severe Amblyopia
Background and Study Questions
When patching is chosen to treat amblyopia, there has been much controversy among pediatric ophthalmologists regarding the dose of patching to prescribe. Some practitioners have prescribed as little as 1 hour a day, whereas others have prescribed as much as 24 hours a day. In severe amblyopia (20/100 to 20/400), regimes at the more intense end of the spectrum have typically been prescribed. Nevertheless, there has been ongoing debate regarding the necessity of full-time patching. Therefore, an RCT was conducted to compare prescribed full-time patching (all or all but 1 waking hour a day) with prescribed 6 hours of daily patching.4
Patients Included in the Study
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree