Summary
A variety of tumors, both benign and malignant, can be found in the orbit of the pediatric patient. This chapter elaborates on the different tumors in terms of diagnosis and treatment as on the various different surgical approached that can be used in treating these tumors.
25 Orbital Surgery for Tumors
25.1 Introduction
Orbital tumors in children are quite rare. Most tumors are benign, mainly cysts; 1 however, malignant and life-threatening tumors 2 can also occur. In this chapter we discuss the common orbital tumors as well as the possible surgical management options.
25.1.1 Benign Tumors
Orbital Cysts
Orbital cysts are the most common benign tumors in the pediatric population. Such cysts can be primary or secondary, congenital or acquired, and may have diverse etiologies such as post-surgical, traumatic, inflammatory, or idiopathic. 1
Dermoid and epidermoid cysts are the most common benign cysts in the orbit. These are choristomas that originate from aberrant ectodermal tissue and are located between two suture lines of the skull that close during embryonic development. Approximately 50% of dermoids involving the head are found in or adjacent to the orbit, either in the supero-temporal or, less commonly, in the supero-nasal aspect of the orbit. 1 These lesions are usually superficial but may also be deep in the orbit. Surgical removal is the treatment of choice, usually held after the age of 1 year. During surgery, care should be given for a complete removal of the cyst without capsule rupture which might lead to local inflammatory response (▶ Fig. 25.1).

Lacrimal duct cysts are cystic lesions that arise from the lacrimal duct epithelium. They appear as a mass in the lacrimal fossa. Caution is required during surgery to avoid damage to the lacrimal duct. Using intra-lesional dye such as indocyanine green allows complete resection of the cyst with its capsule. 3
Vascular Lesions
Vascular orbital lesions are classified according to pathogenesis, histopathology, and hemodynamic properties. The primary classification is according to the flow within the tumor. High flow malformations contain arterial aneurysm, arteriovenous fistula, and arteriovenous malformation (varices). These lesions usually mandate therapy using invasive radiology with coiling or sclerosing agents. Lesions classified as low flow can be further classified as simple lesions, including venous malformations such as cavernous hemangioma and capillary hemangioma, and lymphatic malformations, such as lymphangioma, which can be macrocystic, microcystic, or mixed. There are also combined lesions, some venous dominant and some lymphatic dominant. 4 , 5
Capillary hemangioma is the most common pediatric vascular lesion, usually presents early in life with decreased vision, limited ocular motility, proptosis, or cosmetic disfiguration. Management of capillary hemangiomas changed dramatically with the use of systemic beta blockers, making surgery less common in these tumors today and is reserved to non-responsive tumors, or cases with severe cosmetic disfiguration (▶ Fig. 25.2). 6

Lymphangioma is a type of low-flow malformation, rarely pure lymphatic, but on most occasions mixed with a venous component. Most cases can be managed conservatively with only follow-up. In cases of cosmetic or medical indication, treatment should be held. 5 , 7 Treatment of such lesions is challenging and consists of excision and drainage of the lesion with the use of sclerosing agents to allow hemostasis.
In most cases only partial resection is achieved, and recurrence is common. 4
Tumors of Neural Origin
Optic nerve tumors in the pediatric population are different from adults both clinically and histopathologically. Optic nerve glioma is the most common optic nerve tumor in children (~4% of all orbital tumors). It usually presents at the age of 4 to 5 years. More than half of patients have neurofibromatosis type 1 (NF1). Usually no treatment is required due to the slow growing nature of the tumor. In cases of CNS or chiasmatic involvement, radiation therapy should be initiated. Surgery is reserved for anterior tumors that impair vision or cause a cosmetically significant proptosis. 8
Other benign tumor of a neural origin, also frequently found in the pediatric population, is plexiform neurofibroma. This tumor is common in NF1 patients and is usually located on the temporal side of the upper eyelid, causing an S-shaped lid. These tumors may cause the S-shape upper eyelid and ptosis that may lead to amblyopia. In such cases surgical treatment is indicated promptly. A surgical approach combining ptosis repair with tumor debulking and upper eyelid reconstruction may result in a significant cosmetic and functional improvement, however, tumor recurrence in common. 9
Schwannoma is an uncommon tumor in the orbit, especially in children, originating from the myelinproducing Schwann cells. They involve mostly sensory nerves as V1 and V2 but can also involve motor nerves and the globe itself. Treatment of such tumors is usually surgical with recent reports advocating adjacent radiotherapy. 10
Osseous Lesions
Benign osseous lesions may also present in the pediatric population. These include fibrous dysplasia and juvenile ossifying fibroma. These lesions can present as a mass with osseous expansion (e.g., fibrous dysplasia) or as a lytic and sclerotic lesion (e.g., juvenile ossifying fibroma). Fibrous dysplasia is an abnormal growth of immature fibro-osseous tissue in the bone marrow, replacing the normal osteoblasts. It is slow growing and usually requires no treatment unless pressing the optic nerve or causing severe proptosis. Juvenile ossifying fibroma is a yellow-white mass filled with cystic spaces. The treatment of choice is surgical excision. 11 Some tumors may secondarily involve the orbital bones such as dermoid and epidermoid cysts and leukemia. 9
Osteoma is a benign, slow growing tumor originating from any bone. It commonly arises from the paranasal sinuses and is usually asymptomatic. It appears as sclerotic, dense, well-defined mass. Surgical intervention is required to alleviate pressure on important orbital structures or to improve cosmetic appearance. 12
Langerhans cell histiocytosis (LCH) is a spectrum of three syndromes in which immature dendritic cells of bone marrow origin proliferate. Eosinophilic granuloma, one of these syndromes, is common in children younger than 4 years, and is the most common expression of LCH in the orbit. It causes proptosis, ptosis, or an enlargement of the palpebral fissure. It most often occurs in the supratemporal frontal bone, where bone marrow is abundant. LCH causes an osteolytic, yellow-colored, hemorrhagic lesion. Treatment consists of surgical excision and sometimes chemotherapy. The other two syndromes, Lettere–Siwe disease and Hand–Schuller–Christian disease rarely affect the orbit (▶ Fig. 25.3). 11

25.1.2 Malignant Lesions
Rhabdomyosarcoma is the most common malignant orbital tumor in children and accounts for about 5% of tumors. It is a mesenchymal soft-tissue tumor, and its orbital presentation accounts for approximately 25 to 35% of head and neck rhabdomyosarcoma and around 10% of all rhabdomyosarcoma. The orbit may also be involved by spread of mesenchymal tumors from the nasopharynx, pterygopalatine fossa, or paranasal sinuses. 7 Orbital rhabdomyosarcoma arises most frequently adjacent to the extraocular muscles. 13 It usually occurs in the superior part of the orbit and causes rapidly progressive proptosis with globe displacement and possible motility restriction. About 85% of all orbital rhabdomyosarcoma are of the embryonal type which has a 5-year survival rate (5YSR) of approximately 95%. Other types are the alveolar which is a more aggressive type with a 75% 5 year survival rate and an affinity for the inferior orbit, and the pleomorphic and butteroid types which are much less common in the orbit. 14
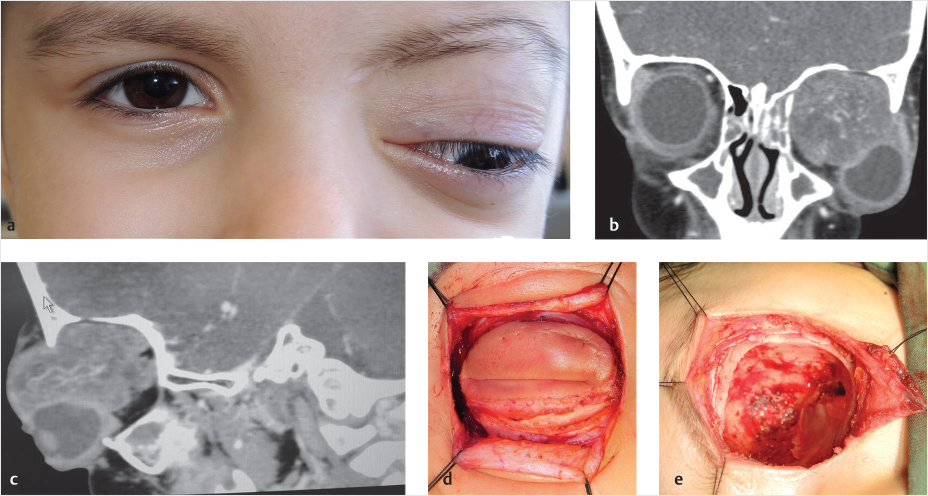
Therapy nowadays consists of systemic chemotherapy with local external-beam radiation therapy. Surgical intervention has remained mainly for tissue diagnosis and for the treatment of repeated tumors after failure of conservative treatments. In some cases, exenteration may be usually required (▶ Fig. 25.4). 14 , 15
Retinoblastoma, an intraocular malignant tumor, may spread through the optic nerve into the intracranial optic tracts and the subarachnoid space. 8 Only 2% has extraocular invasion including scleral, extrascleral, and optic nerve. The presence of orbital retinoblastoma is indicative of an advanced disease, appears around the age of 3 years, usually with proptosis (70–85%), redness, swelling, and pain. Diagnosis includes imaging and total-body scanning for metastases. Vast changes in the detection of such tumors along with genetic consultation have improved survival to 88–93%. Current treatment regimens, after systemic evaluation for metastases, include the use of systemic or local chemotherapy (including intra-arterial melphalan) and local external beam radiation. 16 In cases of massive orbital involvement, exenteration may be required.
Osseous malignant tumors in children include osteosarcoma, chondrosarcoma, and Ewing sarcoma. Osteosarcoma induces bone destruction and osteoid production. Treatment consists of surgical excision and chemotherapy. 11 Ewing sarcoma is the second most frequent, extraorbital tumor to involve the orbit. It is usually located in long bones and treatment is by surgery, chemotherapy, and radiation (▶ Fig. 25.5).

Orbital metastases are quite rare and usually indicate neuroblastoma elsewhere in the body. Neuroblastoma includes metastases to the orbit in 28 to 33% of patients. It usually involves soft tissue and can lead to proptosis but the main site of involvement is the orbital bone. 17 Other malignant tumors found in the orbit in pediatric populations are leukemia, which can be intra- or extraocular, and to a less extent, lymphoma.
Pediatric lesions may involve any part of the orbit and the clinical work-up in conjunction with complete history and appropriate imaging, as specified in the next section, dictate the surgical approach for treatment of these lesions (▶ Table 25.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


